When dealing with frequent headaches, you might not consider the connection between your jaw and migraines, but understanding "how chewing system inflammation can trigger migraines" is crucial. Inflammation in the chewing system, particularly in the jaw muscles and joints, can lead to significant discomfort and even provoke migraine episodes. This article explores the link between jaw inflammation and migraines, shedding light on why addressing dental health is vital for those suffering from chronic headaches.
Key Takeaways
- Inflammation in jaw muscles can activate the trigeminal nerve, triggering migraines.
- Common triggers include stress, poor posture, and teeth grinding.
- Signs of jaw inflammation include jaw pain, headaches, and difficulty chewing.
- Treatments include physical therapy, medications, and lifestyle changes like stress management.
- Seek professional help if jaw pain persists or headaches worsen.
Understanding Inflammation in the Jaw
Navigating the complexities of jaw inflammation reveals a critical connection between the chewing system and migraines. Those tiny muscles in the jaw can wreak havoc if inflamed due to overuse or stress. Ever experienced that dull, relentless headache after a long day of clenching your jaw? That could be the culprit.
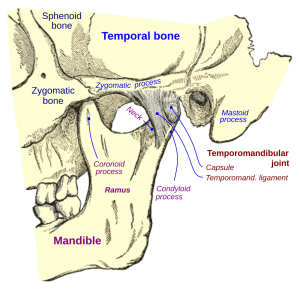
Chronic stress often fuels this inflammation, demonstrating how chewing system inflammation can trigger migraines and lead to a cascade of discomfort. Imagine the jaw muscles as a stubborn knot that refuses to untangle, causing tension headaches. Add teeth grinding into the mix, and it's like throwing fuel on a fire. The key players here are the chewing muscles, particularly the temporalis, which can become overworked.
But why should we care about these stubborn muscles? Well, the answer lies in the pain pathways. The trigeminal nerve, a major player in pain transmission, gets involved when inflammation strikes. This nerve doesn’t just sit idly by; it loves to send fiery signals straight to the brain.
So, what's the takeaway? Addressing inflammation in the jaw isn't just about comfort; it's about preventing those dreaded migraines, which can knock you off your feet. It's vital to tackle the root cause before the migraines tighten their grip.
How Inflammation Affects the Nervous System
When exploring how chewing system inflammation can trigger migraines, it becomes clear that inflammation touching the nervous system can set off a cascade of discomfort. The trigeminal nerve becomes a key player, transforming minor irritations into full-blown migraines. Imagine it as a mischievous messenger, overreacting to every little signal. The inflammation doesn't just tap on the shoulder of this nerve; it gives it a hearty shake.
This nerve, sensitive to disturbances, can become overactive, firing off pain signals like a faulty alarm system. It's like a chain reaction, where one small spark can lead to a massive blaze. Inflammation from the jaw muscles, especially, can be the catalyst, sending the trigeminal nerve into overdrive.
Ever wondered why migraines seem to come out of nowhere? Sometimes, it's the daily grind of stress and tension in the jaw. Picture stress as the villain, sneaking up and tightening its grip. It's no wonder migraines leave people clutching their heads.
Reducing inflammation might be the secret weapon. Think of it as defusing a bomb before it explodes. By calming the inflammation, we can keep the trigeminal nerve from wreaking havoc, offering a reprieve from the relentless migraines.
Key Signs of Chewing System Inflammation
Understanding how chewing system inflammation can trigger migraines can help you spot the telltale signs early, saving you from a world of pain. Jaw discomfort, headaches, and struggles with chewing are common red flags. You know that feeling when your jaw pops or clicks? That’s not just an odd quirk; it could be a warning sign.
Stress or bad posture often ups the ante, so if your headaches spike after a hectic day, your jaw might be to blame. When your jaw feels tender, it's like a pesky reminder that something's not quite right.
Ever had one of those days where your head pounds like it's a rock concert? That could be your body telling you that your jaw inflammation is stirring trouble. The link between chewing and migraines is as real as it gets.
So, next time your jaw acts up, it might be worth considering its role in those relentless headaches. Imagine it like a domino effect: one misstep, and suddenly everything's tumbling down.
Keep an ear out for those clicking sounds. They’re often your body’s way of waving a red flag. If they persist, maybe it's time to check in with a professional.
The Connection Between Jaw Inflammation and Migraines
The relationship between jaw inflammation and migraines is like a complex chain reaction. This inflammation can irritate the trigeminal nerve, setting off a cascade of pain signals straight to the brain. It's as if your jaw's own personal chaos decides to throw a party, and your head didn't get the memo. The nerve's heightened sensitivity to inflammation turns minor jaw aches into full-blown migraine episodes, complete with debilitating pain, nausea, and aversion to light and sound.
When you think about 'how chewing system inflammation can trigger migraines,' consider how stress-induced grinding or clenching of teeth can intensify the issue. It's almost like your jaw is the unruly neighbor, causing disturbances well beyond its borders.
These disturbances can become habitual, with stress and poor posture playing supporting roles in this unfortunate drama. If you've noticed more frequent migraines after a tense day, your jaw might be the hidden culprit.
Keep in mind that your body sends signals; those persistent jaw pains and headaches are not just background noise. Ignoring them is like turning a blind eye to a ticking time bomb. Seeking help from a healthcare professional can illuminate the path to relief.
Role of the Trigeminal Nerve in Migraines
Understanding how the trigeminal nerve plays into migraines reveals a complex narrative. This nerve, with its three branches, is like a highway for pain signals from the face and scalp to the brain. Inflammation within the chewing system can turn this nerve into an overly sensitive alarm, leading to migraines. Imagine it as a smoke detector going off at the slightest hint of smoke; that’s how this nerve reacts to inflammation.
Stress and parafunctional habits, like teeth grinding, act as triggers, setting off a chain reaction that ends in debilitating pain.
Imagine the trigeminal nerve as a vigilant guard, always on high alert. It's good at its job, maybe a little too good. When inflamed, even minor triggers can cause it to raise a red flag, culminating in intense migraines.
Migraines can be as stubborn as a mule, often striking at the worst times. They come with a band of accomplices: nausea, light sensitivity, and sound sensitivity. Understanding the role of the trigeminal nerve in this painful orchestra helps in strategizing effective treatment.
Ultimately, knowing how chewing system inflammation can trigger migraines opens avenues for targeted interventions.
Common Triggers of Chewing System Inflammation
Understanding how chewing system inflammation can trigger migraines starts with recognizing the common triggers, such as stress and poor posture. Stress can lead to muscle tension, which, in turn, causes inflammation. Maintaining a relaxed jaw can be as tricky as balancing plates on a stick. Stress isn't the only culprit; poor posture is another sneaky trigger. Slouching at your desk or hunching over your phone puts undue pressure on your jaw.
Parafunctional habits like teeth grinding are serious troublemakers, especially at night. Imagine waking up with sore jaw muscles as if you've been chewing bricks in your sleep. Incorrect bite alignment is another factor that can turn your jaw into a battlefield. It forces your muscles to work overtime, leading to inflammation.
These triggers can snowball, leading to increased jaw muscle activity. This can activate the trigeminal nerve, turning minor aches into full-blown headaches or migraines. Awareness of these triggers helps in managing inflammation and reducing migraine attacks. If stress is your constant companion or slouching your favorite pastime, think about ways to counteract these habits. Small changes can make a big difference in keeping your chewing system inflammation in check and your migraines at bay.
Effective Treatments for Reducing Inflammation
Exploring how chewing system inflammation can trigger migraines highlights the importance of reducing inflammation with targeted treatments. A mix of approaches focuses on relieving stress on the jaw joint. Physical therapy can be particularly beneficial, offering exercises to strengthen and relax the jaw muscles. This not only alleviates tension but also helps correct posture, which is often a contributing factor. Medications, including muscle relaxants or anti-inflammatories, provide relief by addressing acute pain and reducing inflammation.
Dental orthotics might seem like a stretch, but they offer immense support by correcting bite alignment. This reduces strain, preventing excessive wear and tear on the jaw muscles. For more persistent cases, Botox injections have shown promise. They work by temporarily paralyzing overactive muscles, reducing muscle contractions that contribute to inflammation.
Lifestyle changes can also play a significant role. Stress management techniques, such as mindfulness or yoga, can keep tension at bay. Good posture, often overlooked, can make a world of difference. Regular exercise and a balanced diet help maintain overall muscle health, too. It’s all about making small adjustments that collectively add up to significant improvements. Just remember, sometimes the simplest changes pack the most punch in managing inflammation and its related symptoms.
Lifestyle Changes to Prevent Jaw Inflammation
Understanding how chewing system inflammation can trigger migraines emphasizes the importance of making daily habit changes to prevent jaw inflammation. Let’s uncover some practical strategies. First off, stress management is key. Incorporating relaxation techniques, like deep breathing or meditation, can reduce tension that might otherwise tighten those jaw muscles.
Equally important is maintaining good posture. Imagine your head as a bowling ball; keep it aligned to avoid unnecessary strain. This helps not only the jaw but the entire neck and back as well. Another sneaky culprit causing inflammation is gum chewing. Consider swapping it out for healthier habits. Your jaw will thank you!
Diet also plays a role. Foods rich in omega-3 fatty acids, like salmon or walnuts, help reduce inflammation. Stay hydrated, too. Water is the oil that keeps your body’s engine running smoothly.
Exercise isn't just for the body; your jaw can benefit from gentle stretches and exercises. These can improve function and reduce stiffness over time.
Finally, listen to your body. If you sense discomfort, pause and assess. Early awareness can prevent bigger issues down the road. Remember, small tweaks in habits can create a ripple effect, ensuring a healthier, pain-free life.
When to Seek Professional Help
If you’ve learned how chewing system inflammation can trigger migraines, you'll understand the importance of taking persistent jaw pain seriously. If jaw pain lingers like an unwelcome guest or headaches become relentless, it's time to consider outside expertise. Early action is your best friend here. Trust me, waiting won't make it vanish. If chewing becomes a chore or the jaw refuses to cooperate, seeking professional guidance could save you from future headaches—literally.
Ever notice how migraines sneak in after a particularly stressful day? Your jaw might be a culprit. Don't wait until you're in over your head. Catching symptoms early could mean the difference between a quick fix and a long road of discomfort. A healthcare professional can diagnose the nuances your mirror can't reveal.
Feeling like you're stuck in a loop of throbbing pain? Break the cycle. Your quality of life is too valuable to be compromised. The right professional intervention could be the missing puzzle piece. They bring the expertise to identify underlying issues and offer tailored solutions. But remember, this isn't about just any help—find someone who understands the intricate dance between jaw inflammation and migraines.
Don't leave your comfort to chance; sometimes, a little nudge from a professional is all it takes to turn the tide.
Managing Chewing System Inflammation with Raleigh Facial Pain
In conclusion, inflammation in the chewing system can play a significant role in triggering migraines, making it essential to address any underlying dental or jaw issues. Understanding this connection can lead to better migraine management and overall well-being.
For expert care in diagnosing and treating chewing system inflammation, trust the specialists at Raleigh Facial Pain. Our comprehensive services for chewing system inflammation are designed to alleviate discomfort and help you manage migraines effectively. Let Raleigh Facial Pain guide you toward lasting relief and a pain-free life. Contact us today to know more.