"PAINS" in head & neck region are complex structures, complex mind body interplay, and develop in unique series causing increase intensity of pain and adaptation of pain system. The only force that can influence body to heal is a team professionals.
How can you hope a doctor selling the latest fad in medicine like botox, ARS, or guru's magic potion could solve your pain problems ? I know you are too busy to mess with this pain demands any more than broken leg, but pain will steal your happiness.
As teen or early 20's we develop pain #1, say it is tension headaches (HA). As we enter college or work force, we develop pain #2 say neck pain. Now as woman with two children-house-career-social-ole yes-husband, we develop pain #3, say restricted opening or atypical toothache. With women's 36 hour day or man's 28 hour day, we reach point when quality of our life is in jeopardy.
The word "PAINS" are typically structural damage or infection or inflammation that is additive until the pain system is reaches an overload of signals.
NECK
EARS
FACE
HYOID
NERVE
HEAD
TOOTH
SINUS
VASCULAR
JAW JOINT
Chronic Overlapping Pain Conditions (COPC):
HEADACHES:
HEAD PAIN:
A source of pain coming from the head area, unilateral or bilateral, moderate-severe, episodic-daily-constant, can be pure Ten HA-migraine or Mix HA, may have symptoms with other special organs like eyes, ears, joint, teeth.
Adolescents with migraines and tension HA have higher emotional liability and lower self-esteem.
MIGRAINE HA = NEUROLOGIST
TENSION HA = OROFACIAL PAIN SPECIALIST MIXED HA = OROFACIAL PAIN & NEUROLOGY
Headache Categories & Prevalence: 1. Tension Headache: 48% females, 38% males 2. Migraine Headache: 18% females, 8% males
Tension Headache:
Mixed Headache are mixtures of tension and migraines. They present as whole head headaches or bilateral temple HA. They are moderate to severe. They are mixtures dull-ache with spikes of throbbing pain. They are frequent episodic or daily. They may have mild photo-phono as post headache symptom when headache severe. No aura (no visual effect before onset headache). Most have cervical dysfunction.
Migraines are accumulation multiple source inflammation in head & neck region. Migraines are severe throbbing pounding whole head headaches. Migraine specialist are neurologist.
Orofacial specialist may assist neurologist treating migraine by reducing massive inflammation load coming from chewing system. All headaches reduce frequency, severity, and duration after chewing system orthopedics.
30% to 50% of population have neck inflammation-damage-pain that affects their quality of life.
In 22 of 25 post-whiplash cases, articular disc disorder was diagnosed (tearing lateral ligament TMD)
Weinberg & Lapointe 1987. J Oral Max Surg 45:653
Motor Vehicle Accident: Sudden acceleration deacceleration of condyle will tear lateral ligament of the temporomandibular joint and tear ligaments of cervical region.
WHIPLASH illustration: Showing effect TMD
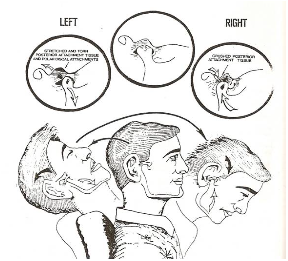
Whiplash in ER: Did you know Jaw Joint gets damaged as do necks in car accidents. in a study where they took MRI on series of whiplash injuries, 22 out of 25 of the TMD's had disc displacement.
NECK PAIN: A source of Inflammation muscles and joints of neck, special structures in neck, can be unilateral or bilateral, can be Mild-moderate-severe, can be Episodic-daily-constant
TALE TWIN SISTERS: following an motor vehicle accident:
Cervical muscles
10% to 15% population suffer from jaw joint pain & dysfunction impairing their chewing system and affecting quality life.
Progression of Disc displacement:
Tearing of lateral ligament of disc:
Sports-Related Injuries & TMD:
Certain blows to jaw with right force and direction can tear the lateral ligament to jaw joint
FALL: produces whiplash injuries like tearing to LATERAL LIGAMENT OF TMD DISC
CHEWING SYSTEM DAMAGE:
RESTRICTED OPENING REFERRAL
Dental appliances are not effective on moderate damage muscle joint complex of jaw joint. (Biteguard, Nightguard, Anterior Repositioning Splint, LVI appliance, OLMS, NTI -anterior deprogrammer)
A general dentist may treat muscle pain or mild damage TMD (partially displaced disc), but if there is moderate damage to TMD, they need to be refer to orofacial pain specialist for chewing system orthopedics.
Moderate Damage requires team health care professionals:
Dentist & hygienist choose refer restricted opening to Orofacial Pain Specialist due complex of problem and complexity of joint.
Anesthesilogist with a report of history restricted opening or restricted at time exam, need to refer Orofacial pain specialist to provide healing to TMD so intubation can be provided w/o post operative jaw pain.
Atypical Toothache= 7 % to 12 % of all toothaches are not pulpal origin
Atypical toothache: HINTS
Inside nerve verses outside nerve:
For anyone so brave and ego centric to think this is always clear, you need to go to endodontist or orofacial pain specialist office to shadow to learn the art of diagnosis difficult cases and respecting the level difficulty.
Diagnostic tree for atypical toothache
Symptoms Atypical Earache
Jaw joint complex is the 2nd most likely cause ear discomfort
Neuralgia, Neuritis, Neuroma 5th Cranial Nerve
Impulses through damage nerve:
Complexity nervous system, pain system and chewing system sets stage for complexity of Orofacial Pain team to manage the annoying-ongoing-relentless-nerve pain.
Orthotic is diagnostic tool for reducing impulses through trigeminal nerve.
Discomfort in face associated w/ inflammation in outside nerve of upper tooth near maxillary sinus causing confusion between sinus and tooth causalgia.
Hints/Symptoms:
HYOID SYSTEM: a source of pain coming from mostly inflammation from hyoid system, includes inflammation from suprahyoid and subhyoid muscles unilateral or bilateral, mild-moderate-severe, episodic-daily-constant,
UPPER RESPIRATORY SYSTEM: Allergies, VIrus/Bacteria, Sensitivities, Airway Mannagement; any source of inflammation coming from the tissues in direct contact with outside world, interaction with lymph tissue and immunity systems sets up inflammation,
Swallowing is hint of hyoid system dysfunction. Airway restriction is cause of hyoid dysfunction Odd symptoms associated w/ hyoid accompanies many TMD cases w/ little science for diagnostic efforts.
Forward position of hyoid system & mandible is set up by small air pipe. The positioning of the hyoid system forward drags the tongue out of the air pipe and the muscle that must do work is Lateral Pterygoid that displaces disc in TMD. Make matters worse for displace disc some dentist are using ARS appliances on purpose to open airway. Even if this looks good for airway, it will increase the number displaced disc or increasing the TMD in world.
Some patients brace the mandible in forward position to pull the tongue out airway when they have a severe airway problem. This is adaptation required for survival, but it is not an improvement on health of joint. Another form of parafunction and parafunciton damage the jaw joint disc complex.
Look to future of science in discovering many of these observations that are more clinical, but these are seeds to research direction in future.
"PAINS" in head & neck region are complex structures, complex mind body interplay, and develop in unique series causing increase intensity of pain and adaptation of pain system. The only force that can influence body to heal is a team professionals.
How can you hope a doctor selling the latest fad in medicine like botox, ARS, or guru's magic potion could solve your pain problems ? I know you are too busy to mess with this pain demands any more than broken leg, but pain will steal your happiness.
As teen or early 20's we develop pain #1, say it is tension headaches (HA). As we enter college or work force, we develop pain #2 say neck pain. Now as woman with two children-house-career-social-ole yes-husband, we develop pain #3, say restricted opening or atypical toothache. With women's 36 hour day or man's 28 hour day, we reach point when quality of our life is in jeopardy.
The word "PAINS" are typically structural damage or infection or inflammation that is additive until the pain system is reaches an overload of signals.
NECK
EARS
FACE
HYOID
NERVE
HEAD
TOOTH
SINUS
VASCULAR
JAW JOINT
Chronic Overlapping Pain Conditions (COPC):
HEADACHES:
HEAD PAIN:
A source of pain coming from the head area, unilateral or bilateral, moderate-severe, episodic-daily-constant, can be pure Ten HA-migraine or Mix HA, may have symptoms with other special organs like eyes, ears, joint, teeth.
Adolescents with migraines and tension HA have higher emotional liability and lower self-esteem.
MIGRAINE HA = NEUROLOGIST
TENSION HA = OROFACIAL PAIN SPECIALIST MIXED HA = OROFACIAL PAIN & NEUROLOGY
Headache Categories & Prevalence: 1. Tension Headache: 48% females, 38% males 2. Migraine Headache: 18% females, 8% males
Tension Headache:
Mixed Headache are mixtures of tension and migraines. They present as whole head headaches or bilateral temple HA. They are moderate to severe. They are mixtures dull-ache with spikes of throbbing pain. They are frequent episodic or daily. They may have mild photo-phono as post headache symptom when headache severe. No aura (no visual effect before onset headache). Most have cervical dysfunction.
Migraines are accumulation multiple source inflammation in head & neck region. Migraines are severe throbbing pounding whole head headaches. Migraine specialist are neurologist.
Orofacial specialist may assist neurologist treating migraine by reducing massive inflammation load coming from chewing system. All headaches reduce frequency, severity, and duration after chewing system orthopedics.
30% to 50% of population have neck inflammation-damage-pain that affects their quality of life.
In 22 of 25 post-whiplash cases, articular disc disorder was diagnosed (tearing lateral ligament TMD)
Weinberg & Lapointe 1987. J Oral Max Surg 45:653
Motor Vehicle Accident: Sudden acceleration deacceleration of condyle will tear lateral ligament of the temporomandibular joint and tear ligaments of cervical region.
WHIPLASH illustration: Showing effect TMD
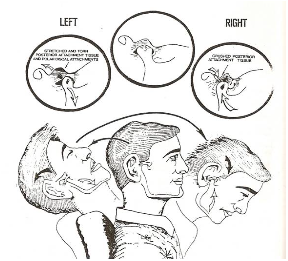
Whiplash in ER: Did you know Jaw Joint gets damaged as do necks in car accidents. in a study where they took MRI on series of whiplash injuries, 22 out of 25 of the TMD's had disc displacement.
NECK PAIN: A source of Inflammation muscles and joints of neck, special structures in neck, can be unilateral or bilateral, can be Mild-moderate-severe, can be Episodic-daily-constant
TALE TWIN SISTERS: following an motor vehicle accident:
Cervical muscles
10% to 15% population suffer from jaw joint pain & dysfunction impairing their chewing system and affecting quality life.
Progression of Disc displacement:
Tearing of lateral ligament of disc:
Sports-Related Injuries & TMD:
Certain blows to jaw with right force and direction can tear the lateral ligament to jaw joint
FALL: produces whiplash injuries like tearing to LATERAL LIGAMENT OF TMD DISC
CHEWING SYSTEM DAMAGE:
RESTRICTED OPENING REFERRAL
Dental appliances are not effective on moderate damage muscle joint complex of jaw joint. (Biteguard, Nightguard, Anterior Repositioning Splint, LVI appliance, OLMS, NTI -anterior deprogrammer)
A general dentist may treat muscle pain or mild damage TMD (partially displaced disc), but if there is moderate damage to TMD, they need to be refer to orofacial pain specialist for chewing system orthopedics.
Moderate Damage requires team health care professionals:
Dentist & hygienist choose refer restricted opening to Orofacial Pain Specialist due complex of problem and complexity of joint.
Anesthesilogist with a report of history restricted opening or restricted at time exam, need to refer Orofacial pain specialist to provide healing to TMD so intubation can be provided w/o post operative jaw pain.
Atypical Toothache= 7 % to 12 % of all toothaches are not pulpal origin
Atypical toothache: HINTS
Inside nerve verses outside nerve:
For anyone so brave and ego centric to think this is always clear, you need to go to endodontist or orofacial pain specialist office to shadow to learn the art of diagnosis difficult cases and respecting the level difficulty.
Diagnostic tree for atypical toothache
Symptoms Atypical Earache
Jaw joint complex is the 2nd most likely cause ear discomfort
Neuralgia, Neuritis, Neuroma 5th Cranial Nerve
Impulses through damage nerve:
Complexity nervous system, pain system and chewing system sets stage for complexity of Orofacial Pain team to manage the annoying-ongoing-relentless-nerve pain.
Orthotic is diagnostic tool for reducing impulses through trigeminal nerve.
Discomfort in face associated w/ inflammation in outside nerve of upper tooth near maxillary sinus causing confusion between sinus and tooth causalgia.
Hints/Symptoms:
HYOID SYSTEM: a source of pain coming from mostly inflammation from hyoid system, includes inflammation from suprahyoid and subhyoid muscles unilateral or bilateral, mild-moderate-severe, episodic-daily-constant,
UPPER RESPIRATORY SYSTEM: Allergies, VIrus/Bacteria, Sensitivities, Airway Mannagement; any source of inflammation coming from the tissues in direct contact with outside world, interaction with lymph tissue and immunity systems sets up inflammation,
Swallowing is hint of hyoid system dysfunction. Airway restriction is cause of hyoid dysfunction Odd symptoms associated w/ hyoid accompanies many TMD cases w/ little science for diagnostic efforts.
Forward position of hyoid system & mandible is set up by small air pipe. The positioning of the hyoid system forward drags the tongue out of the air pipe and the muscle that must do work is Lateral Pterygoid that displaces disc in TMD. Make matters worse for displace disc some dentist are using ARS appliances on purpose to open airway. Even if this looks good for airway, it will increase the number displaced disc or increasing the TMD in world.
Some patients brace the mandible in forward position to pull the tongue out airway when they have a severe airway problem. This is adaptation required for survival, but it is not an improvement on health of joint. Another form of parafunction and parafunciton damage the jaw joint disc complex.
Look to future of science in discovering many of these observations that are more clinical, but these are seeds to research direction in future.

1) Sensitivity:
a) Early sensitivity = biteguard
b) Mod sensitivity…
 Raleigh Facial Pain © 2024 All Rights Reserved.
Raleigh Facial Pain © 2024 All Rights Reserved.