A child will get jaw joint damage if the grind/clench, anxiety, or traumas are significant enough at an early age. A gifted pedodontist keeping up with latest science can add hypermobility and poor sleep to the mix of damaging factors setting up potential for displaced disc in young person.
Referral Orofacial Pain Specialist 1) Tension Headache 2) Destructive Parafunction 3) Disc Displacement 4) Airway Protection & Braces 5) Juvenile Rheumatoid arthritis
PEDIATRIC TENSION HEADACHE
THE QUESTION: Why is my child in pain???
As a parent, it is difficult to see your child w/ frequent moderate to severe headache and have nothing to offer them. We feel helpless, hopeless, and frustrated that science has not given provided primary care physicians any safe treatments for children headaches, but most importantly as parent, we want to control the pain and suffering.
FIRST ANSWER:
- Majority of headaches in children are “Tension Headaches”.
- Tension headache is pain in chewing muscle called Temporalis
- If the headaches are frequent or severe enough affect quality lifed
- Parents are confused on who seek care for headaches
- Referral to Neurologist for headaches using strong medications
- Strong medications have not been tested on children HA
- Specialist treating muscles and joints of TMD is Orofacial Pain Specialist
- Orofacial pain specialist uses Integrative tools to manage Tension HA
Pediatric Tension Headache: A child w/ tension HA is most likely a clencher or grinder w/ moderate anxiety.
Why Referral orofacial pain: HA disrupts school-social-sleep: Because you care for suffering of child 1) Escalates to severe 2) Becomes daily 3) Ibu is causing IBS 4) Grades dropping 5) Child irritability increase 6) Recent blow head, MVA, Fall 7) Increase anxiety, stress 8) breaking fillings, retainers, crowns 9) Poor sleep
Moms in conflict
- Suffering w/ pediatric headache
- Use medications not tested on children
- Specialist manages child's headache
Good news Orofacial Pain Specialty management of Pediatric HA:
- pediatric headaches reduced in frequency, severity, and duration
- Majority tools are Integrative tools
- Integrative tools target reduction inflammation
- All forms of inflammation are targeted
- Requires team health care professionals
- Patient and parent are part of team
- Secret success is in patient passion for health
- Team leader, coach, science teacher is orofacial pain specialist
Pedodontics & Destructive Bruxism
Diagnosing destructive grind-clench in child is critical to reducing suffering in child from tension headache: 1) Wear teeth: focus on 1st molar for indication 2) Broken retainers, spacers, pedo crowns, fillings 3) Severe wear on Invisalgin or Hawleys or other appliances 4) Look past teeth at enlarged muscles or clicking TMD
3 levels of grind-clench:
1) Mild 2) Moderate 3) Severe (destructive)
What is destructive parafunction ?
- Movement disorder
- Restless mouth syndrome
Misconceptions: Grinding-clenching: No concern
- Wear on baby teeth
- Hearing your child grind at night
- Grinding one level of damage
- Grinding is bad habit
Destructive Parafunction (grinding/clenching):
- frequency, power, and duration are high
- Most damage is done at night
- Power can go up 6 times daytime power
- Damages all 4 chewing structures
- Damage to jaw joint & muscles difficult tx
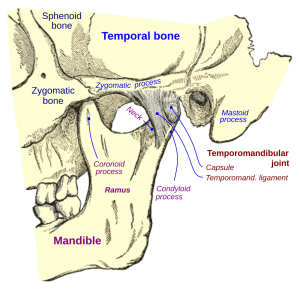
- TMD -TMD refers to when joint-muscle are damage
- Destructive grind requires Pedodontist and mothers diagnose
Why refer destructive parafunction to Orofacial Pain Specialist ?
- Pain is Not from tooth damage
- Pain is from Joint muscle damage
- Destructive grind is Not bad habit
- Destruct grind is Movement disorder
- Destructive grind cannot be managed w/ just biteguard
- Destructive grind is manage by team utilizing 11 tools
- Destruct Grind Cannot be cured
- Destruct grind can only Reduce to nondestructive level
Parafunction is destructive force behind pedodontics failures
- Broken filling
- Broken Hawley
- Worn out Invisalign
- Broken nightguard
- Broken retainers
- Moderate wear 1st molar
- Sensitivity
- Failed SSC-pulpotomy
- Mobile teeth-moving teeth
- Retainers discomfort (tight) in evening
When does grinding & clenching become destructive?
- Grinding power goes up 6 times chewing power
- Power-duration-frequency elevated
- High anxiety-constant or frequent, moderate level
- Significant interferences or bite problems
Retainers are adequate in controlling tooth movement after braces in mild & moderate parafunction, but they are woefully inadequate in destructive parafunction.
Single tools are inadequate for managing destructive bruxism. In fact destructive grinders, can break night guards when only single tool is utilized.
Why is destructive grinding-clenching difficult diagnose and refer?
- Not looking at chewing system as whole
- Not collect hints from 4 different areas
- Examine more than teeth: collect hints from bone, muscle, joint, airway, bite, appliances, spacers
- Chewing system is fragmented into areas interest
- Dental specialties do not communicate well
- Destruction joint & muscle not taught dental school
- Insurances do not allow enough time to collect data
- Hammer see nails, plumber sees pipes, dentist see teeth
- Most pedodontist are over whelm with data and care they already covered
Pedodontics complex case like Tension Headache, Displace Disc TMD, or Destructive Grind-Clench
- Research chronic pain (our training was acute pain)
- Determine chronic pain early as possible
- Expand data collection for chronic pain
- Educate parents to understand destructive nature grind-clench
- Petition insurance & government insurance remove time constraints for chronic pain
- Diagnose destructive parafunction & refer early possible
- Refer orofacial pain specialist
Disc Displacement in children
Pedodontist should manage muscle damage chewing system or even mild level damage to TMD with conservative therapie for chewing system.
Can moderate TMD damage (complete disc displacement) occur in children: Yes. Because it is not prevalent, many are mistaken to think it will not happen in young people.
What look for Moderate TMD damage
- Chewing pain
- Tension Headache
- Moderate Wear 1st molar
- Frequent jaw joint noises
- Deviation opening
- Restricted opening
What are causes disc displacement in children : 1) Destructive grinding 2) Traumas 3) Tension in Muscles 4) High anxiety
Why does restorative dentistry cause sensitivity or discomfort in moderate jaw joint damage?
- Jaw joint instability affects position & integrity of teeth
- Jaw joint Instability causes ever changing bite
- Dual bites must be discovered before orthodontics
- Braces can increase jaw pain or complete displacement disc
Orthodontic exam should now include: 1) Airway analysis Class II 2) Tongue size vs arch size 3) Palatal extension 4) Size Medial Pterygoid 5) Sleep apnea 6) TMD damage level 7)Parafunctional level. 8) Anxiety level
In complete disc displacement, a child needs a chewing system orthopedic team:
- Diagnose complex case
- Understand orthopedic team and responsibilities
- Prepare treatment plan including 3-4 months orthopedics
- Coach for success and provide latest in science mom & child
- Refer when need chewing system muscle joint specialist
Complexity of each case: 1) Cardio conditioning 2) GI issues. 3) Use stimulants 4) Different pains 5) Level grind 6) Anxiety wires pain system 7) Types trauma 8) Sleep quality. 9) Anxiety level
Child has moderate jaw joint damage, mom needs seek referral w/ orofacial pain specialist.
Orofacial pain specialist: 1) team leader 2) coach 3) science educator 4) guide 5) facilitator 6) assist team 7) help patient set goals 8) pain manage coordinator
Chewing system Orthopedic Team: 1) Patient 2) Physical Therapy 3) Biofeedback 4) Orofacial Pain Specialist 5) Pedodontist 6) Allergist 7) ENT
Levels Damage TMD: 1) Mild = Partial Disc Displacement. 2) Moderate = Complete Disc Displacement 3) Severe = Osteoarthritis
When would you see severe case in child ? Rheumatoid Arthritis.
With that said, all rheumatoid cases should be referred to have grind-clench evaluated to prevent arthritis from setting up damage of Childs TMD. Protect their eatability.
Pediatric Airway Management
The great Pedodontist of today takes into account the airway needs of patient when planning any treatment plan especially Class II case or small air pipe case. Never allow an orthodontist or pedo orthodontist to pull premolars to shrink lower arch because it shoves tongue into air pipe.
Walls of air pipe:
- Palatial
- Side walls
- Tongue vs arch size
Side wall made up of
- Medial Pterygoid
- Tonsils
- Pharyngeal wall-skin-connective tissue-fat
Lower wall: 1) tongue vs arch discrepancy, 2) Large tongue 3) Small arch 4) Mandibular Tori 5) Palatal width & depth 6) Palatal tori 7) Posterior Crossbites
Premolar extraction w/ braces:
- Standard of care in past
- Did not ask about snoring-sleep breathing
- Test for sleep apnea
- Analyzes airway walls
- Small airway should never premolar extract, reduce arch size, reduce tongue space, & shove tongue into airway
- Consider re-bracing for increase arch size, even with spacing
Airway management:
- Collect data on sleep breathing
- Collect data on snoring
- Collect data on quality
- Test for sleep apnea
- Analyzes arch verses tongue size discrepancy
- Analyzed palatal extension
- Analyze size Medial Pterygoid
- Consider fat content in walls back throat
The problem w/ premolar extraction:
- arises when we treat all patients with same approach and we do not take into account the other oral needs like breathing. Some of our past care, violate the needs of airway. A person with small pipe reducing size of arch pushing tongue into airway would set up snoring problem.
Why refer Pedodontist:
- Complex cases: should only be done by a well-trained pedodontics, study of complex cases requires keeping up latest in sciences
- Simple to moderate cases managed by general dentist w/ adequate training is implemented
Quote: “I can teach you how to do root canal in weekend, but it takes 3 years to teach the exceptions.”