Trigeminal Nerve Pains
- Trigeminal neuralgia
- Burning mouth
- 5th Neuralgia & Neuroma
NERVE DAMAGE: Trigeminal Nerve; The nerve of Orofacial Pain Specialist
Nerve Pathologies Orofacial Pain Specialist can help relieve pain if the nerve is trigeminal nerve.
- Trigeminal neuralgia
- Neuroma
- Neuritis
- BMS
- Neurovascular
- Intracranial compression
- Nerve Entrapment
- Extracranial compression by growth
Therapies for trigem:inal nerve 1. Nerve blocks a. Auriculotemporal b. Infraorbital c. Supraorbital 2. Topicals 3. Neuropathic medications 4. Chewing system orthopedics
Burning Mouth:
- if there is any hope of getting better, the patient must accept that anxiety is critical to manage.
- There is not quick fix.
- There is no way around biofeedback and counseling.
- There is no way around use neuropathic medications.
- There is no cure only proper management to level that you have a quality life.
- We have had a few patients that totally relieved the burning pain, but that is exception.
- Do not call expecting miracles, we are fresh out.
- If you want to work harder than you have ever worked on anything, then feel free to call.
- Burning mouth is the most difficult pain to treat in field orofacial pain specialist.
- Anxiety, emotional hyjacking, PTSD, child abuse are the focus of most of the therapy
- Care at RFPC team is directed at a. Reduction of inflammation sources in head n neck b. Reduction in stress and anxiety
BMS Statistics:
- 5% population
- Tip togue & ant palate
- Female (4 to 1)
- 5th to 7th decade
- Pain in trigeminal nerve
- Absence trauma-event-infection-causalgia
- Can have taste changes
Trigeminal Neuralgia
When the trigger is near oral region, it requires Orofacial pain specialist to differentiate between tooth pathology & TN, due it’s ability to mimic pathologies of the chewing system.
Presentation: 1. Cluster of episodes 2. Severe pain 3. Electric or shock 4. Unilateral attacks 5. Triggered by touch, wind, brush, gum
Concerns:
- TN can look like severe toothache
- Neurologist must rule out dental pathology
- Dentist must rule out TN; so, refer OFPS
- Dentist refer to Orofacial pain specialist to solve riddle
- TN is cross over pathology (Medical to Dental) in head
Trigeminal Neuralia resembles
- Toothache 2) Jaw pain 3) Facial pain 4) Gum-Bone pain
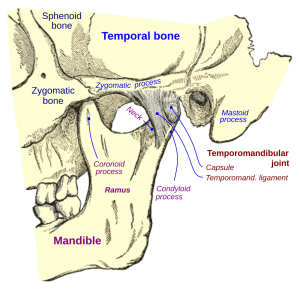
Diagnostic Confusion w/ TMD:
- Many TN patient’s have moderate TMD damage
- TMD and TN nerves are part of trigeminal nerve
- TN pain is managed first, then the TMD pain
- Mixture of TN & TMD pains confuses diagnosis
Diagnosis of TN:
- intensity of pain
- pattern of the pain
- no dental pathology
are the most effective symptoms for diagnosing TN
Trigeminal Neuralgia is so painful: 1) Prompt dentist or Endodontist to do emergency root canal 2. Emergency referral to Orofacial pain specialist
Trigeminal Neuralgia:
- Pulsating artery lengthens w/ age, rubbing insulation off top of trigeminal nerve, allowing moderate impulse to jump into pain fiber w/ low impulse, setting off electric shock
- Increase probability w/ age due lengthening of in cranial arteries
Management of Trigeminal Neuralgia:
- Anticonvulsants
- Mircovascular Decompression
HEADACHE: Confusion between migraine & tension headache?
The majority headaches are tension headaches. Majority headaches in women. Majority women between 30 to 50.
Headaches Champions
MIGRAINE = NEUROLOGIST
TENSION HA = OROFACIAL PAIN SPECIALIST
Orofacial Management HA:
- Tension HA: side head muscle is Temporalis, a chewing muscle, refer orofacial pain specialist
- Mixed HA: combinations migraine & tension HA
- OFP Treats Tension HA to separate out that HA, then refer neurologist
- Neurovascular HA: Atypical Odontalgia
- Migraine: refer neurologist
Headache Categories & Prevalence: 1. Tension Headache: 48% females, 38% males 2.Migraine Headache: 18% females, 8% males
Tension Headache: can be episodic--frequent--daily, Unilateral temple or bilateral temples More frequent women Mild: Dull, ache; Moderate: throbbing; Moderate to High levels anxiety; Worse upon awakening or as day progress on workdays
Mixed Headache: components tension and migraine, Severe whole head (bilateral temples), Frequent episodic or daily, May have mild photo-phono post HA, No aura (no visual effect before onset HA), Most have cervical dysfunction
Migraines are thought to be accumulation multiple source inflammation in head & neck region. Migraines should be referred to neurologist. If neurologist needs assistance from orofacial pain due tension headache or mixed headache with tension HA component.
Orofacial specialist may assist neurologist treating migraine by 1. Reduction cervical inflammation 2) Reduction in parafunctional muscle contraction 3) Reduction inflammation in Temporalis muscle (side head 4) Reduction in tension in muscles from anxiety-stress 5) Improved healing muscle joint by sleep therapy