SURGICAL GUIDELINE: Surgery is indicated only in severe damage TMD (arthritis) and only arthrocentesis.
RECONSTRUCTION GUIDELINE: 1) Reconstruction should never be performed before establishing TMD Stability by Chewing System Orthopedic team. 2)Reconstruction is should never be performed before the force of DESTRUCTIVE GRIND-CLENCH is reduced.
ENDODONTIC GUIDELINE: If a root canal does not relieve pain in tooth, request Orofacial Pain Testing for other 6 reasons for ATYPICAL TOOTHACHE.
PEDODONTIC GUIDELINE: If a child presents with frequent headaches, requesting a Orofacial Specialist evaluation for Tension Headache is considered best care for child.
PEDODONTIC PREVENTION GUIDELINE: If we could observe some early hints of destructive grinding and refer Chewing system orthopedics, we can save patient a lot pain, tooth destruction, tension headaches, and anxiety.
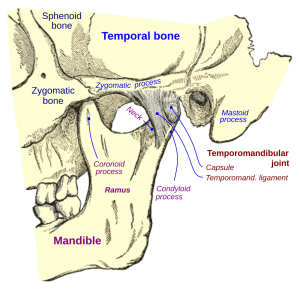
Three types surgery for TMD:
- Meniscus Plication Surgery
- Arthrocentesis
- Jaw Joint Replacement
Mencius Plication Surgery (MPS) Indications: 1) Chewing system orthopedics fails reduce pain to acceptable level 2) Damage completely displaced disc w/o recapture 3) New research improves outcome. 4) Orofacial pain specialist controls factors before surgery
Mencius Plication Surgery (MPS) discontinued in 1990's due:
- By not controlling the damaging factors
- Pull SLP tore suture line
- Orofacial pain specialist were not available in control factors
- Surgeons were able to improve other joint systems
TMD surgery: Arthrocentesis:
- Flushing jaw joints to remove cartilage - bone fragments - inflame chemicals
- Assist orofacial pain specialist to heal arthritic cases -- removing rock in shoe
- Used in severe pain arthritic cases
Braces are deferred until stabilization jaw joint in jaw locking- moderate jaw pain-high anxiety cases.
Orthodontic Exam for TMD stability:
- Determine TMD Damage
- Chewing pain
- History locking
- Facial Asymmetry
- Moderate-severe wear
Moderate damage:
- Restricted opening
- Chewing pain
- Bite changes
Braces are not a treatment for TMD
- Braces can increase jaw pain
- Braces can cause pain flares
- Bite is not stable in complete displaced disc
- Where does orthodontist place teeth, if bite is changing
- RULE THUMB: jaw joint stability before brace
Can orthodontist determine moderate damage to jaw joint ? 1) They can get feel for moderate damage by collecting symptoms and using their knowledge chewing system 2) Not usually, patient's rarely report previous lockings-pain-noises-bite problems-traumas w/o skill interviewer 3) Patient rarely observe grind/clench in sleep or sense how tense their muscles have become 4) Sensing anxiety increases pain after long periods time in pain is rare talent in patients 5) Patients with high pain threshold rarely report severe pain, "hidden OA can have milld pain"
When a patient develops episode of jaw pain or restricted opening during braces, it reveals hidden moderate damage to jaw joint, typically complete displaced disc.
What causes jaw pain during braces? ( Undiscovered or hidden ) 1) Complete Disc Displacement 2) Osteoarthritis
Braces tx major occlusal problems after jaw joint stability is re-established
- After treating moderate to severe jaw joint damage
- Establish ideal occlusion to prevent future TMD damage
- Major interferences are concern in grinding teeth
- Braces establish more stable bite
If jaw pain or restricted opening develops during braces:
- Hint of moderate damage in jaw joint
- Time out on braces for 1 month
- Orofacial Pain Team recruited
- Passionate control damaging factors
- Promote healing by changing health habits
- Re-start orthodontic therapy
Periodontics, bone loss-recession-pockets are blamed on bacterial infection and little attention to mechanical destruction of support to teeth.
By placing all grinding-clenching in same box, the destructive grinding/clenching (a movement disorder) causing severe destruction of support for teeth (Perio) is all but ignored as caused by occlusion.
Periodontist are highly trained at bacterial damage to support to teeth, but mechanical damage from destructive parafunction is training is limited. Like rest dental profession, we focus on teeth rather the destructive force behind damage to chewing system, "destructive parafunction".
Hints destructive parafunction
Enlargement bone Recession w/o disease Mobile teeth
Bone loss w/o disease Restricted opening Microfractures
Sensitivity Cracks Broken teeth
Discomfort teeth Mod-Sev wear Jaw clicking
Tension HA Enlarge Masseter Broken NG
Buccal bone buttressing Lower buccal bone buttressing Upper lingual bone enlargement
Bone loss w/o infection hints destructive parafunction
Early destructive grind-clench preserves valuable resources of mouth to prevent periodontitis
Dentist treat sensitivity as recession issue with chemical desenstization, but mechanical irritation to outside nerve and ligament causes most of sensitivity.
Course of sensitivity treatments at dental office:
- Dental tx sensitivity:
- paint tooth w/ cavity varnish or fluoride
- adjust occlusion 1 tooth
- Grafting
- Repetitive sensitivity necessitates look at destructive parafunction
- Nightguard
- Occlusal adjustment
- Paint Sensitivity
- Recession
- Cervical erosion filling
Occlusion
- TMD causes bite changes, more than occlusion causes TMD
- Symptoms destructive parafunction,referOrofacial Pain Specialist
- Tool available to periodontist is nightguard
- Nightguard is great tool to reduce parafunction damage to support teeth
- Orofacial Pain Specialist has 10 more tools to control destructive parafunctional disease
Treat symptoms destructive parafunction w/ Nightguard
- Avoidinterferences
- Slow recession
- Prevents future Bone loss
- Splint mobile teeth
- Protect bone support
- Reduces propagation of cracks
- Preserve tooth structure
- Reduces periodontal damage
Treat destructive parafunction
- Occlusal adj treats interference but not power causing damage
- Occlusal adjustments reducesdamage interference causes
- Occlusal adjustments slows down parafunctional damage
- Occlusal adjustments can help manage single tooth discomforts
When Endodontist tackle the ATYPICAL TOOTHACHE, the most complex and confusing diagnosis on planet. if there ever was a "damn if do and damn if don't" predicament it is the decision of whether the outside nerve or inside nerve is cause of your pain.
Atypical Toothache
- Toothaches w/o caries near inside nerve tooth (pulp)
- Suspect irritation to outside nerve of tooth
- Refers Orofacial pain to differentiate the6 other causes AT
- Orofacial Specialist is Diagnostic clearinghouse for atypical toothache
- Helps patients save their teeth from chasing tooth pain ghost
- Primary AT is hidden destructive parafunction damaging outside nerve
Referral: 1) oral surgeon for Crack tooth 2) Endodontist if inside nerve 3) Refer orofacial pain specialist if outside nerve 4) Orofacial pain specialist if it is central nerve 5) Orofacial Specialist if you are not sure cause
of outside nerve-ligament