
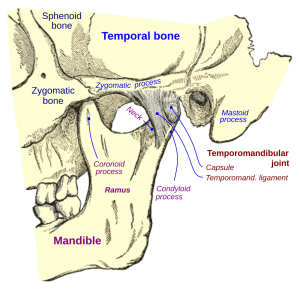

In short, an orofacial pain specialist is a board certified and residency trained doctor. Orofacial pain management requires a combination of medicine and dentistry to accurately diagnose, treat, and relieve chronic orofacial pain in muscles, joints, and nerves of the chewing system.
Our pain center:
We once treated a woman who suffered an oral burning pain for over six months. After initiating treatment and eliminating her pain, her husband came to us saying, “Thanks for giving my wife back to me.” There are many such occasions to celebrate at the Raleigh Facial Pain Center and these are also the most satisfying moments in our practice – to join with people to visualize and then realize a life that is pain free.
60% referred from dentistry, 40% referred from medicine; 70% referred by general dentists and doctors, 30% referred by specialists
Medical insurance — joint muscle therapy is a part of the body like any other joint
Court rulings, the insurance commissioner, and the law all declare services associated with joint, muscle, and nerve conditions be listed under medical care. Anything directly related to tooth treatment is listed under dental. Orofacial pain treats muscles, joints and nerves only.
Yes. Orofacial pain services are treated the same way as other orthopedic services (back, legs, neck, etc.).
The female predisposition to chronic pain is at a 3 to 1 ratio of female to male, according to double-blind random studies. The primary reasons are related to estrogen, hypermobility and stress.
These patient were orphans
Why would an ENT not refer you to a general dentist? Unfortunately, the general dentist is inadequately trained in dental school for chewing system damage (TMD or TMD). Even a general dentistry professional who has taken weekend courses will tell you that the complexity of the chewing system is too much for weekend training. For you see, chewing system orthopedics is more than mouthpieces, more than pain medication, more than simple home remedies. Trust me, while practicing dentistry in the mountains, after extensive weekend courses, I could not handle the complexity of TMD, TMD or chewing system damage.
Dentists like Dr. Yount attend a 2-3 year orofacial pain residency and become board certified in orofacial pain. This two-three year residency provides extensive training in medical, dental, and allied health professions. The specialty of orofacial pain covers the areas of treatment that falls between the dental and medical fields. Orofacial pain is a blend of the medicine and dentistry sciences. The complexity of TMD-TMD requires knowledge of all sciences as well as tooth and joint dynamics to ensure successful pain management.
General dentists provide care in the area of bruxing (tooth wear). A few general dentists will provide care for simple chewing muscle pain of short duration and low pain levels if there is little to no jaw joint involvement (deviation, restriction, facial asymmetry, painful click, etc) and no significant medical complications (fibromyalgia, lupus, sleep disorder, arthritis, etc). In other words, the general dentist with extra training can diagnose and manage early simple cases of MPD (inflammation of chewing muscles), as well as some early cases of partial disc displacement of short duration, but does not usually treat moderate or complex TMD. Some cosmetic dentists attempt to treat facial pain but have not been thoroughly trained or board certified. Be leery of procedures and therapies that are not reversible.
Over 95% of pain pathologies are acute pains, while the other 5% is chronic pain. Chronic pain is defined as pain lasting longer than one month with multiple aggravators or initiators sensitizing the pain reporting system. If you’ve tried a one-time treatment such as medication, bite appliance, or soft diet and it has not worked or worked well, it is time to consider that your pain may be chronic.
most cases it is waste money, it is usually too bulky to wear comfortably, does not treat chewing pain, and makes grinding worse
In the past, dentists thought bite was the cause of MPD/TMD (TMD). Now bite or occlusion is recognized as only one of the minor factors. Thus, braces will likely not help, considering the bite is only a small part of the problem. Based on a study, 1/3 of patients get worse, 1/3 stay the same, and 1/3 get better using braces to solve the TMD/TMD problem. This means that 2/3 of patients do not get a pain reduction
No. This open mouth procedure can make your pain significantly worse. The crown procedure is based on a patient’s bite being stable, but the bite is not stable with TMD/TMD. The jaw joints are being stabilized on slick inclines and the muscles are in different contraction vectors and forces. The dentist will not be able to get the crown, bridge, partial or implant comfortable, while open mouth procedures can make TMD/TMD far worse.
Less than 3% of TMD cases require arthroscopic surgery to rinse the joint out. The open joint surgery is not done at the present time because it failed us in the past.
An orthotic is the only appliance that is backed by science for treatment of TMD/TMD. It:
No ,surgery is off line at moment in time. Besides, when there is conservative therapy that is highly successful, why would you subject your daughter to invasive idea.
Atypical Earache
Destructive Parafunction
Restricted Opening
Pediatric Headache
Tension Headache
Atypical Toothache
Causes of MPD/TMD

 Raleigh Facial Pain © 2026 All Rights Reserved.
Raleigh Facial Pain © 2026 All Rights Reserved.